What Is an Ectopic Pregnancy?
In September 2020, lifestyle blogger Devida Lederle chronicled a devastating event she says she never saw coming “in a million years.” Lederle, creator of multi-channel health and wellness platform The Healthy Maven, wrote candidly about the weeks-long saga that ensued once she discovered her first pregnancy was ectopic.
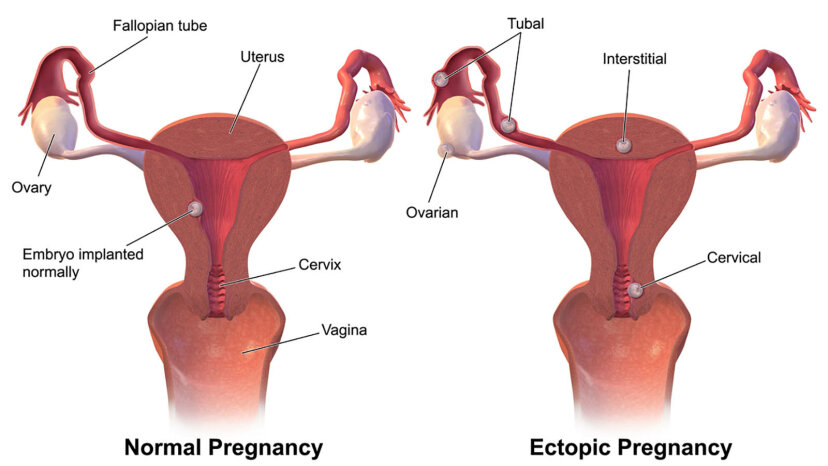
“If you don’t know anything about an ectopic pregnancy, it’s basically a pregnancy that develops outside of your uterus,” Lederle wrote on her blog. “A healthy and viable pregnancy can only develop in your uterus. If it develops elsewhere it is not a viable pregnancy. 2 percent of all pregnancies are ectopic (very rare) and 98 percent of them happen in a fallopian tube. At this point I was in the 2 percent of the 2 percent in that my ectopic could not be found. But it was time to start making decisions and moving forward.”
Lederle dove deep into the details of what ensued after her diagnosis, but despite the increasing number of frank and comprehensive conversations around pregnancy loss and ectopic pregnancies in particular, many people are still unaware of what this condition is really all about.
What Is an Ectopic Pregnancy?
“An ectopic pregnancy is a pregnancy that’s growing in a place other than the womb (or uterus),” explains Katharine White, MD, MPH, assistant professor of obstetrics and gynecology at Boston University. “The most common place for an ectopic to be is in one of the fallopian tubes, but an ectopic can also be in the cervix, on an old cesarean section scar, in the corner (cornua) of the uterus, or on the ovary.”
According to the American College of Obstetricians and Gynecologists (ACOG), almost all ectopic pregnancies — over 90 percent — occur in a fallopian tube. This can have serious and even deadly consequences because as the pregnancy progresses, it can cause the tube to burst, which may lead to major internal bleeding, a potentially life-threatening emergency that requires immediate surgery.
Despite the seriousness of their circumstances and the general lack of candid conversation about them in the public discourse, ectopic pregnancies aren’t as rare as you may think. “Ectopic pregnancies make up about 2 percent of all pregnancies, so I see them in my practice all the time,” White says. “Sometimes we just discover an ectopic when a patient has a routine ultrasound early in pregnancy. But more often, we order an ultrasound when the patient reports spotting or pelvic cramping, particularly on one side of their pelvis. Sometimes we can see the actual ectopic on the ultrasound, and sometimes we know one is there by following the blood pregnancy hormone levels (which don’t rise the way they’re supposed to).”
Fertility expert Aimee D. Eyvazzadeh, MD, MPH, host of “The Egg Whisperer Show,” says she diagnoses about one to two ectopic pregnancies every year. “The ectopic rate is higher in patients doing in-vitro fertilization (IVF),” she says, noting that she uses a five-step fertility check for all patients called “the TUSHY Method” that examines the fallopian tubes, uterus, hormone levels, genetics and the sperm of any male partner.
“This is why I include the ‘T’ [for ‘tube] of TUSHY in the work-up for all my IVF patients,” Eyvazzadeh explains. “If a tube is dilated, inflamed and full of endometriosis, then it can affect implantation and an embryo can get either swept away (implantation failure) or float into the tube and get stuck. A blocked tube won’t be able to push an embryo back into the uterus. I feel like I’m seeing more endometriosis now compared to when I started my practice almost 14 years ago. I think it’s really important for people to know that endometriosis can also block fallopian tubes and increase your risk of an ectopic pregnancy. This is yet another reason why knowing if you have endometriosis is so important.”
What Are the Risk Factors?
Risk factors are a complicated question when it comes to ectopics. Research has offered conflicting findings on the matter, and because every person is unique, there is no guarantee that an ectopic can be traced back to one specific cause. ACOG states that certain conditions and factors, like previous ectopic pregnancy; fallopian tube, pelvic or abdominal surgery; pelvic inflammatory disease; endometriosis; and certain sexually transmitted infections (STIs) can increase the risk for an ectopic. And some factors, like cigarette smoking, age (women older than 35 are said to be at a higher risk), a history of infertility and the use of assisted reproductive technology, like IVF, can increase chances of an ectopic as well.
But in Lederle’s case, the risk factor question was a frustrating one. “At least 50 percent of ectopics have no known risk factors,” she says. “It’s really disheartening as someone who’s had one to see how much they emphasize the risk factors when none of them apply to you! You basically spend your time wondering if you’ve ever had chlamydia and not known it or if that one cigarette you had in college caused it.”
The Mayo Clinic also indicates that women who use intrauterine devices (IUDs) should be aware of the risks when it comes to ectopics. Getting pregnant while using an IUD is extremely rare, but if a pregnancy does occur with an IUD in place, it’s more likely to be ectopic.
“I wish people knew that ectopic pregnancies are common, and that there’s nothing you can do to cause it or to prevent it from happening,” White says. “We also can’t move the pregnancy from the abnormal location into the uterus — patients ask me that all the time.”
What Are the Early Signs and Symptoms?
As Lederle chronicled in her blog post, the first indication that something was wrong in her case was persistent spotting after her period had finished. “… week after my period ‘should’ have been finished I was still spotting and cramping,” she wrote. “I found this unusual and thought I’d just connect with my OB-GYN to be safe. We chatted (pandemic-style) over the phone and she suggested I come in for some testing and that if I had a pregnancy test at home I should use it. I kind of scoffed at the idea because I’d just had my period and thought that unless immaculate conception had occurred there was a 0 percent chance I was pregnant. But I rushed out to CVS anyway and picked up a pregnancy test.”
As Lederle experienced, early symptoms of an ectopic pregnancy include vaginal bleeding or spotting and/or lower belly cramping or intense, constant pain.
The test confirmed that Lederle was, in fact, pregnant, and as she wrote, “we were so happy but also knew that things weren’t adding up so we shouldn’t get too excited.” When she went in for blood work and an ultrasound that afternoon, the tests confirmed that something was off: Her blood tests indicated the presence of human chorionic gonadotropin (hCG), a hormone that is released during pregnancy, yet there was no sign of a pregnancy on the ultrasound. Although her hCG continued to rise over the next two days and she began experiencing the symptoms of early pregnancy (extreme bloating, achy legs, painful breasts, etc.), the ultrasound was still mysteriously clear. “I was officially diagnosed with a ‘pregnancy of unknown location,'” she wrote. “It will likely be the strangest diagnosis I will ever receive in my life. Turns out I was pregnant, they just couldn’t find out where.”
What Are the Risks Associated With an Ectopic Pregnancy?
Ectopic pregnancies aren’t just concerning and confusing — they can be life threatening. “The biggest risk with an ectopic pregnancy is that the site of the ectopic will rupture — your fallopian tubes (and those other non-uterus locations) were not designed to allow a pregnancy to grow safely,” White says. “When rupture occurs, you can bleed so much that you can need blood transfusions. And sometimes a patient bleeds so much that they die. So it’s critical to treat an ectopic pregnancy when it’s found, either by surgery to remove the pregnancy, or by medication to dissolve it.”
Eyvazzadeh says that early diagnosis — like in Lederle’s case — can be a key factor in preventing the more dangerous consequences of an ectopic pregnancy. “This is why every pregnancy is presumed ectopic to a fertility doctor until seen in the uterus,” she says. “With careful management and early diagnosis, patients will do well. They may have to have surgery and have a tube removed but the good news is that you can get pregnant without a tube using IVF. Of course, the bad news is that I just mentioned surgery and the requirement for IVF if you don’t have functioning tubes. The first IVF pregnancy was an ectopic pregnancy. Many people don’t know this fact.”
What Are the Emergency Symptoms of a Ruptured Ectopic Pregnancy?
As Lederle eventually learned first-hand, some ectopic pregnancies rupture. That means the fertilized egg continues to grow in the fallopian tube, causing the tube to burst, triggering heavy abdominal bleeding and potentially life-threatening consequences. Emergency symptoms of an ectopic include:
- Severe abdominal or pelvic pain, along with vaginal bleeding
- Extreme dizziness or fainting
- Pain in the shoulder
After she felt a sharp jab following early treatment for her ectopic, Lederle rushed to the emergency room and underwent surgery, which resulted in the loss of her left fallopian tube.
What You Need to Know for the Future
While ectopics can be devastating, they don’t have to derail a person’s plans to become a parent in the future. “What I wish people knew is that tubal factor is very common [tubal factor infertility occurs when a blockage in the fallopian tube will not allow the egg and sperm to meet],” Eyvazzadeh says. “With the increase in chlamydia rates that we’re seeing (the highest level yet), we will see a rise in ectopic pregnancies too because of the tubal damage that chlamydia causes. My mantra is: the more you know the better things will go. I strongly advocate for women who are starting on their fertility journey to get their tubes checked especially if they have a history of chlamydia. If you have a history of ectopic, ask your doctor for an HSG [hysterosalpingogram: an x-ray procedure that can reveal whether the fallopian tubes are open and if the inside of the uterus is healthy]. If you have a normal HSG and are still not getting pregnant, it’s also possible that your tubes may have scar tissue surrounding them or don’t move properly in order for an intrauterine pregnancy to occur.”
White says that based on her experience in the clinic and having seen countless women endure the emotional fallout of ectopics, she hopes the medical field will evolve to cultivate more empathy and support for patients. “I wish more doctors treated ectopic pregnancies like a miscarriage,” she says. “Sure, they need more medical treatment than a typical miscarriage. But a person can be just as devastated by the loss of a pregnancy in their tube as by the loss of a pregnancy in their uterus.”
Lederle says that her experience with an ectopic pregnancy brought about profound grief — but also immense gratitude. “While I would never wish this experience on anyone, I am forever changed in the way I view pregnancy and having children and this perspective I wouldn’t change for the world,” she wrote. “So now I’m in this club I never wanted to be a part of but especially the ectopic pregnancy club which has so few members. I wish I had more women to talk to about this. So far I’ve had friends tell me about a friend of a friend or a sister who went through this experience but no one who I know personally. My hope with sharing this post is not only to help me heal from my experience but also to connect with other women who have gone through it too.”
This article originally appeared on howstuffworks.com